ABOUT CHRONIC PAIN
Pain is an unpleasant sensation that can range from mild to very severe. People also experience brain injury in a range of severity. Similar to the complex nature of brain injury, pain can be experienced differently from one person to the next. Chronic is the term used to describe pain that lasts for three months or longer. Many of those living with brain injury have chronic pain.
How people manage their pain differs greatly, too. In addition to pain medication options, there are other types of treatment. For example, cognitive behavioral therapy (CBT) with a therapist that can help people to change their thoughts. Planning and pacing one’s activity is another non-medication tool to prevent and manage pain. https://msktc.org/tbi/tbi-topics/chronic-pain-tbi
ACUTE PAIN often results from disease, inflammation, or injury to tissues. It generally comes on suddenly.
CHRONIC PAIN is considered a disease itself (although it may result after injury or illness) and it can be influenced by environmental and psychological factors. It is resistant to most medical treatments. painconsortium.nih.gov
- For every 10,000 PEOPLE with severe pain, there is only ONE BOARD-CERTIFIED pain specialist.
- 20 percent of the adult population suffer chronic pain in the United States, with many experiencing more than one type of chronic pain.
- Chronic Pain is the leading cause of long-term disability in the United States.
- Chronic pain has biopsychosocial implications. It is associated with REDUCED QUALITY OF LIFE, including increased risk of anxiety and depression. uspainfoundation.org
INTERSECTIONALITY WITH BRAIN INJURY
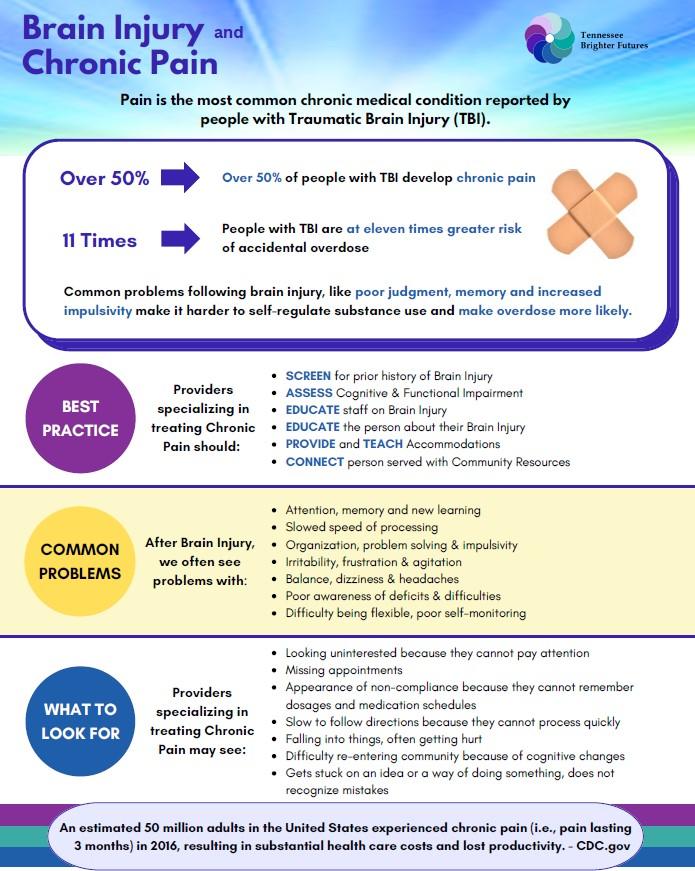
The most common chronic medical condition that people with brain injury report is pain. Over half of people with Traumatic Brain Injury develop chronic pain. Many people have more frequent headaches following injury and they may require medication. People with brain injury are more likely to be prescribed opioids and are at eleven times greater risk of accidental overdose. Common problems following a brain injury, like poor judgment, memory and increased impulsivity, make it harder for them to self-regulate substance use and make an overdose more likely. Pain can make other brain injury symptoms seem worse. The brain injury can make it harder to use pain relief strategies (e.g. exercises, ice packs, meditation, and medication).
People in pain clinics should be screened for prior history of brain injury (especially if the pain resulted from a traumatic event), undergo cognitive screening, be given customized accommodations and referred to community resources as needed. People with TBI may have challenges with auditory comprehension; verbal and written language; reading; social communication; mental health (depression and anxiety) and/or behavior (including anger control issues). These issues may cause problems with understanding of and compliance with treatment.
SCREENING TOOLS
University of Florida, Pain Assessment and Management Initiative, Pain Assessment Scales/Tools
NASHIA’s OBISSS (Online Brain Injury Screening and Support System)
CRISIS INTERVENTION TOOLS
988 Suicide & Crisis Lifeline or you can text to 988; 988lifeline.org to chat with someone
Veterans Crisis Line: Dial 988, then Press 1; or text 838255
NAMI Blog: How to Help Someone in Crisis
211 Helpline | Get Connected. Get Help. (unitedwaygreaternashville.org): The 211 Helpline is a 24/7 365-day information and referral help line that provides individuals in need with help in times of crisis and beyond.
SAMHSA National Helpline: Confidential free help, from public health agencies, to find substance use treatment and information. 1-800-662-4357
NATIONAL WEBSITES
American Academy of Family Physicians (AAFP) Chronic Pain Management Toolkit
U.S. Pain Foundation Resources Infographics, pamphlets, meditations, order free printed resources & more
Model Systems Knowledge Translation Center (MSKTC) Factsheets (1-4) Chronic Pain and TBI and download accompanying Infocomic series (1-4).
Brainline.org articles Managing Pain After Brain Injury & Coping with Chronic Pain
INFOGRAPHICS
National Institutes of Health, Chronic Pain and Stigma Infographic
National Institutes of Health, Pain in America Infographic
U.S. Pain Foundation, Chronic Pain Facts
U.S. Pain Foundation, Our Community Chronic Health Fact Sheet
Advanced Pain Consultants Chronic Pain Facts
National Association of State Head Injury Administrators (NASHIA) Brain Injury and Opioid Overdose: fast facts
PATIENT EDUCATION
University of Florida, Pain Assessment and Management Initiative, Patient Education Activity Book
Mayo Clinic Health System, Pathways through persistent pain: Tips for managing chronic pain
American Psychological Association, How to help a friend or loved one suffering from a chronic illness
HelpGuide.org Chronic Pain and Mental Health
Model Systems Knowledge Translation Center, Traumatic Brain Injury and Chronic Pain Fact Sheet: Part 2
Model Systems Knowledge Translation Center, Headaches after Traumatic Brain Injury Fact Sheet
U.S. Pain Foundation, Medical Cannabis 101 Booklet (not currently legal in Tennessee)
MEpedia Spoon Theory is a way of describing the experience of chronic illness and its limitations using a metaphor
Brain Links’ Personal Guide to Everyday Living After Concussion/Traumatic Brain Injury
TRAINING
U.S. Pain Foundation Pep Talks, Join newsletter and access over 40 webinars
National Association of State Head Injury Administrators (NASHIA) online training
SUPPORT GROUPS
US Pain Foundation Daily Chronic Pain Support Group
Facebook has many online support groups. Search “chronic pain support group.”
TN Brighter Futures groups that are a part of this System of Care:
- Tennessee Society of Interventional Pain Physicians
- Tennessee Pain Society
- Precision Pain Care
Meeting/Training Materials:
Downloadable TBF Chronic Pain Resource Pages PDF
Downloadable TBF Chronic Pain Resource Pages Text File
Downloadable Meeting/Training PowerPoint_Opioids Chronic Pain Damon Dozier, MD with the TN Society of Interventional Pain Physicians