Check out our new TBI Toolkit hub to access Brain Links School Nurses Toolkit:
This playlist was created specifically for School Nurses.
Have you used Brain Links' TBI Toolkit and did you know the CDC Pediatric mTBI Guideline is included? Let us know what you think by completing a short survey!

School Nurses: If an injury is suspected (ie student just fell), recommend using the CDC's Concussion Signs and Symptoms Checklist for School Nurses.
SCREENING FOR PRIOR HISTORY OF BRAIN INJURY:
An abundance of research now clearly shows that people with a prior history of brain injury are more likely to experience problems later in life (beginning as early as one year later). These problems can include: substance misuse, mental health issues, domestic violence (either as the perpetrator or the victim), additional brain injuries, chronic pain, justice involvement, and more. Early identification and ongoing monitoring are, therefore, vitally important.
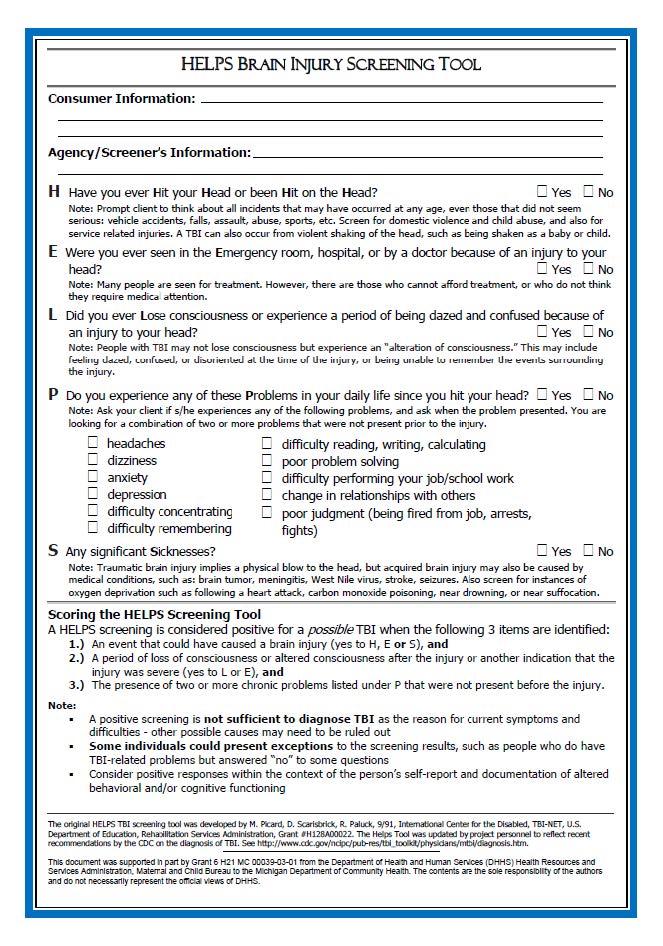
HELPS Brain Injury Screening Tool: The original HELPS TBI screening tool was developed by M. Picard, D. Scarisbrick, R. Paluck, 9/91, International Center for the Disabled, TBI-NET, U.S. Department of Education, Rehabilitation Services Administration, Grant #H128A00022. The Helps Tool was updated by project personnel to reflect recent recommendations by the CDC on the diagnosis of TBI.
- H - Have you ever Hit your Head or been Hit on the Head?
- E - Were you ever seen in the Emergency room, hospital, or by a doctor because of an injury to your head?
- L - Did you ever Lose consciousness or experience a period of being dazed and confused because of an injury to your head?
- P - Do you experience any of these Problems in your daily life since you hit your head?
- S - Any significant Sicknesses?
Yearly screening: Recommend using the HELPS Brain Injury Screening Tool OR add questions to customize the annual health history intake forms.
Example: Circle or provide checkboxes with a space for them to explain.
Ask: Has your child had an injury? Yes No
Cause of injury: Fall Car/motor vehicle accident Sports related other
If Yes: Did your child lose consciousness or become dazed? Yes No Not sure
Please explain: __________________________________________________
Nursing in Non-School Settings:

On intake (and possibly yearly) Brain Link's encourages using the HELPS Brain Injury Screening Tool or consider adding questions to the current intake form.

If an injury is suspected: Brain Links' Nurse's Concussion Screening Checklist. Adapted by Brain Links with permission from the CDC.

This list of resources is shared by the National Association of State Head Injury Administrators (NASHIA)
- Brain Check Survey (BCS):This parent-completed screening tool, from the Life Outcomes after Brain Injury research center within the Department of Occupational Therapy at Colorado State University in Fort Collins, is used to establish a credible history of brain injury. Check out the Brain Check Survey Scoring Tool. Read more from Life Outcomes After Brain Injury Research Program.
- SAFE Child Screening Tool Birth to 3 Years Old: Young children are at high risk for sustaining brain injuries. Data gathered using the SAFE Child Screening Tool will provide information to help professionals develop and implement appropriate services.
- SAFE Child Screening Tool 3 Years Old to Kindergarten: Young children are at high risk for sustaining brain injuries. Data gathered using the SAFE Child Screening Tool will provide information to help professionals develop and implement appropriate services.
- Ohio State University (OSU) TBI Screening Tool: The Ohio State University Traumatic Brain Injury (TBI) Identification Method (OSU TBI-ID) is a standardized procedure for eliciting lifetime history of TBI via a structured interview. Read the full article.
- Ohio State University (OSU) TBI Identification Method — MODIFIED The Ohio State University Brain Injury Identification Method MODIFIED (OSU BI-ID MODIFIED) is a standardized procedure for eliciting lifetime history of any type of brain injury (stroke, tumor, TBI, etc.) via a structured interview.
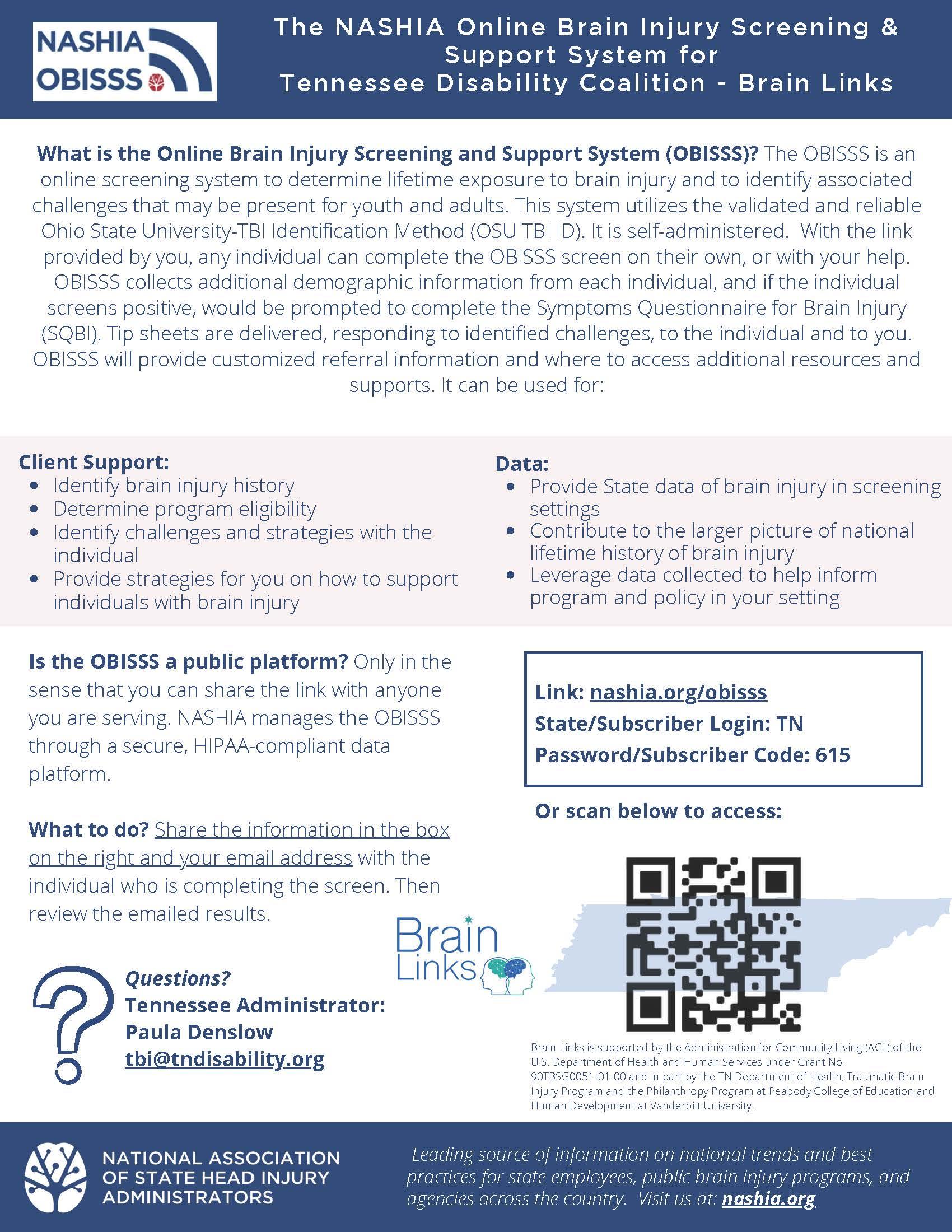
NASHIA's Online Brain Injury Screening and Support System (OBISSS) Tool is a subscription-based screening system that determines a potential exposure to brain injury in someone’s lifetime and identifies any associated problems that are present. Watch the recording of our informational session and view the slide deck for more information.
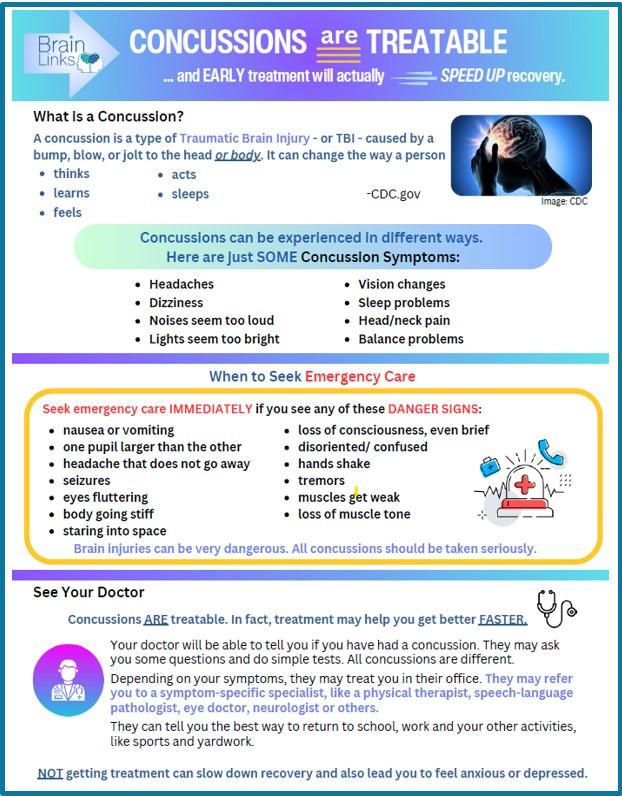
Concussions Are Treatable: In fact, treatment may help you get better FASTER. Your doctor will be able to tell you if you have had a concussion. They may ask you some questions and do simple tests. All concussions are different. Depending on your symptoms, they may treat you in their office. To learn more, explore this resource.
TN TBI Services Directory & Resource Guide: The Tennessee Department of Health Traumatic Brain Injury Service Directory and Resource Information Guide was designed to assist in locating programs, organizations, agencies, and services available across the state of Tennessee and the nation.

TN TBI Service Coordination Program: There are currently eight Service Coordinators (view list) located in various non-profit agencies across the state. The Service Coordinator’s role is to work with persons with brain injury and their family to access current needs. The goal of service coordination is to improve the quality of life for persons with brain injury.
Service Coordination services are provided free of charge, services include:
** develops a comprehensive plan of care;
** provides referrals to available resources;
** coordinates services for individual client advocacy; and
** bridges gaps in the service delivery system.
Virtual and In-person Brain Injury Support Groups have been established across the state. To learn more about services call 1-800-882-0611.

CDC Letter: Returning to School After a Concussion:
DEAR SCHOOL STAFF: This letter offers input from a healthcare provider with experience in treating concussion, a type of traumatic brain injury. This letter was created to help school professionals and parents support students returning to school after a concussion. You can use these recommendations to make decisions about support for your student based on his or her specific needs. This letter is not intended to create a 504 Plan or an IEP unless school professionals determine that one is needed. Most students will only need short-term support as they recover from a concussion. A strong relationship between the healthcare provider, the school, and the parents will help your student recover and return to school.

CDC Factsheet for School Professionals: Returning to School After A Concussion
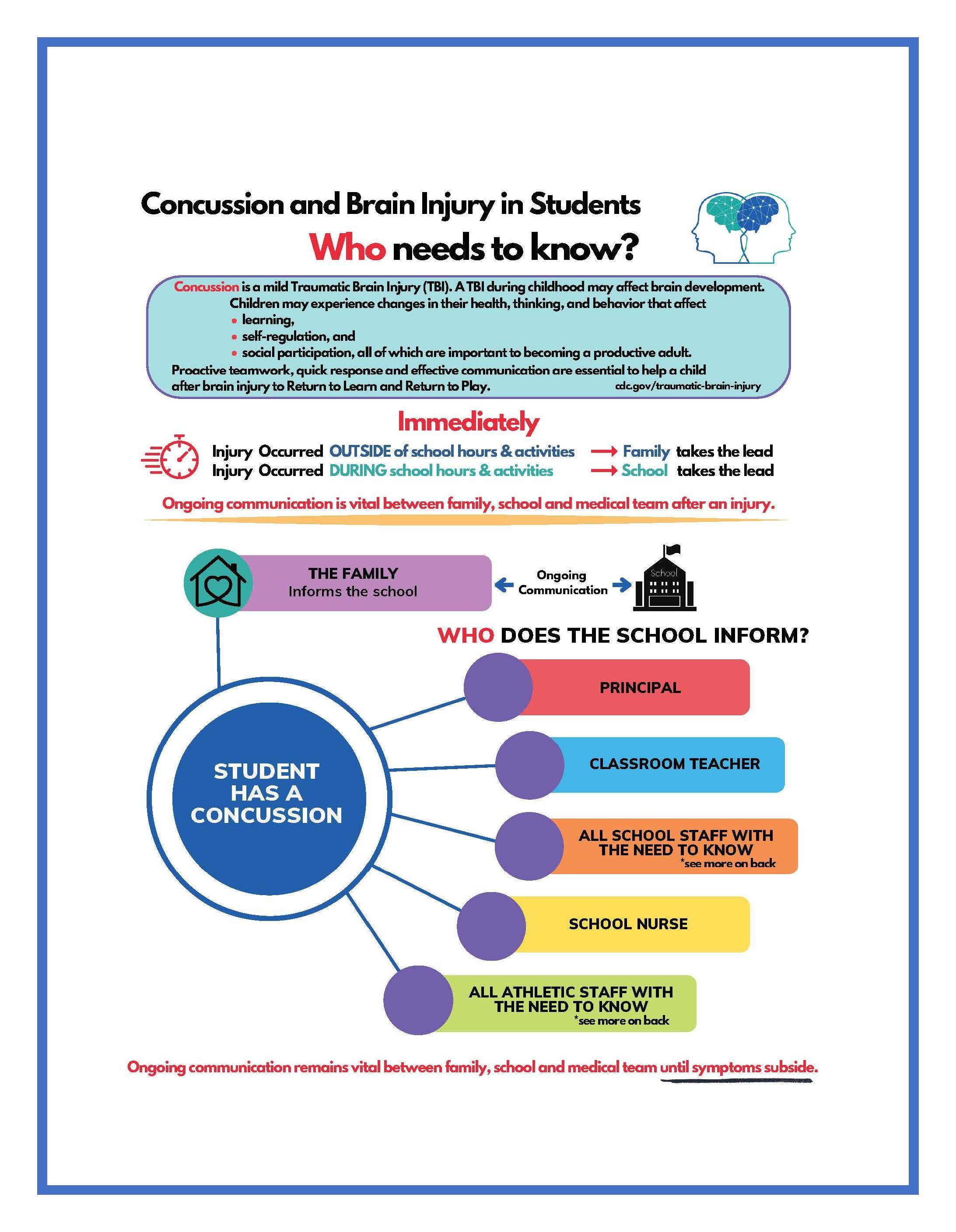
Concussion and Brain Injury in Students, Who needs to know? Concussion is a mild Traumatic Brain Injury (TBI). A TBI during childhood may affect brain development. Children may experience changes in their health, thinking, and behavior that affect learning, self-regulation, and social participation, all of which are important to becoming a productive adult. Proactive teamwork, quick response and effective communication are essential to help a child after brain injury to Return to Learn and Return to Play. cdc.gov/traumatic-brain-injury Word Document File
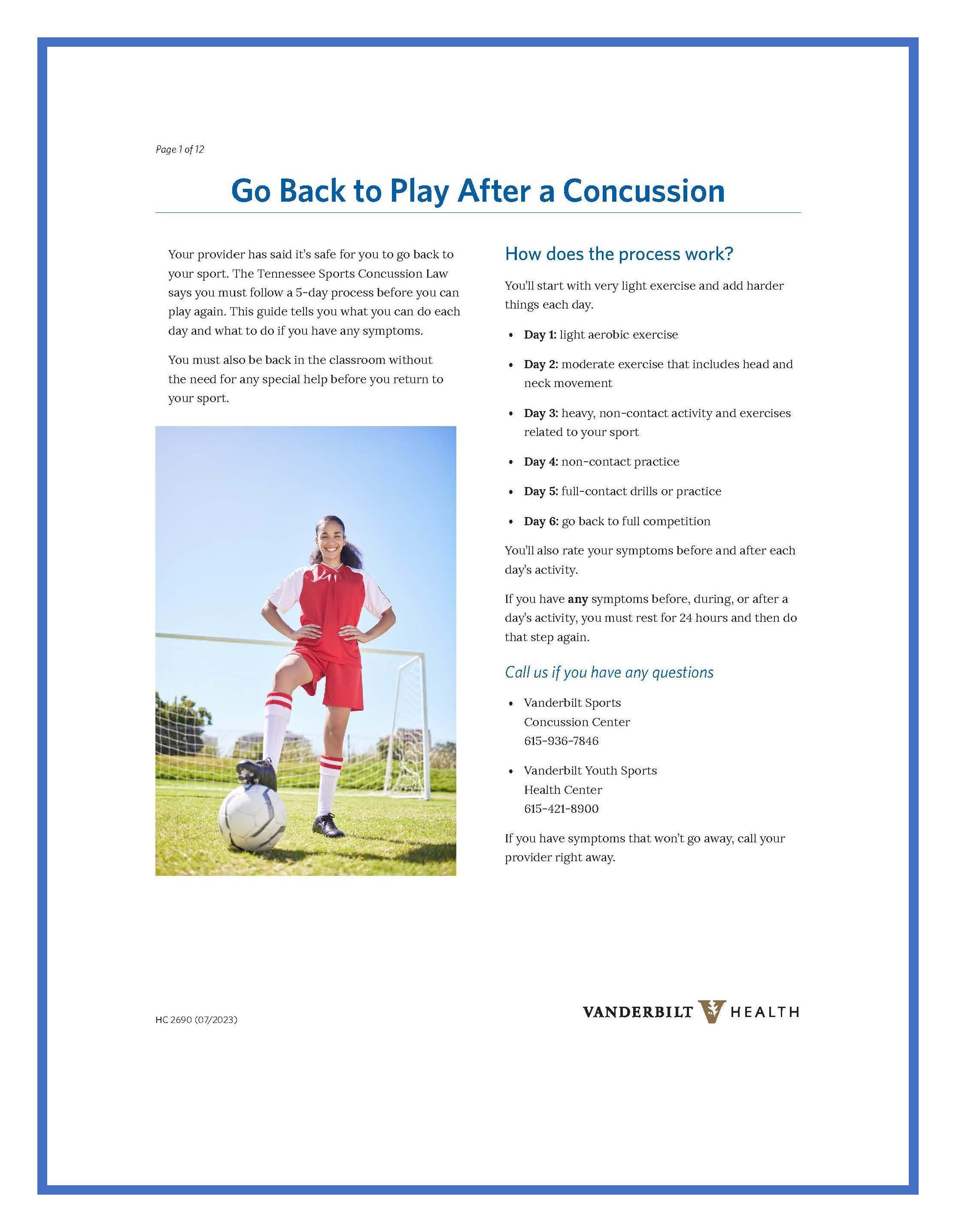
Go Back to Play After a Concussion: This is a concussion return to play manual created for student-athletes who do not have access to an athletic trainer to guide them through the Return To Learn (RTL) process. This manual follows the RTP process required by the Tennessee state concussion law. This resource is a way for parents or coaches to track and document the progress of their athletes. Vanderbilt Sports Concussion Center

Symptom Tracker: Track Symptoms, pain level changes, what provokes and what helps. Good information to take back to the healthcare provider.

Brain Health: How to Have a Healthy Brain Throughout Life: This material provides research-based tips for creating a healthy brain, regardless of age. This guide was originally developed to help people with brain injuries recover to the fullest extent possible and to help them prevent or minimize potential negative changes as they age. However, it was quickly realized that the information in Brain Health is beneficial for everyone. Available in English & Español.

We Can Prevent Childhood Adversity Infographic
A new CDC infographic shows the impact of Adverse Childhood Experiences (ACEs) and how preventing ACEs can help create neighborhoods and communities where every child thrives. This infographic showcases data from the CDC-Kaiser Permanente ACE Study and recent findings to address the following questions:
- What are ACEs?
- How common are ACEs?
- How do ACEs affect our lives?
- How do ACEs affect our society?
- What can be done about ACEs?
ACEs are potentially traumatic events in childhood (0-17 years), such as neglect and experiencing or witnessing violence. However, types of early adversity can be stopped before they start.
Safe, stable, and nurturing relationships and environments have a positive impact in creating positive childhood experiences. Their benefits can last a lifetime.

The HEADS UP to Schools: Online Concussion Training for School Professionals is designed to help classroom teachers (grades K-12), school administrators, paraprofessionals, teachers' aides, and other staff who work with students understand:
- How a concussion may affect a student’s learning, emotions, and behavior.
- How to identify and monitor signs and symptoms of concussion.
- How to help students successfully return to school and recover from a concussion.
This free training will take about 45-60 minutes to complete. It features easy-to-follow information with knowledge checks and illustrated case studies that showcase a variety of scenarios to help you apply the information presented and achieve the key learning objectives of the course.
Check out the CDC HEADS UP Trainings for School and Sports Professionals:
- School Professionals, Youth Sports Coaches, High School Coaches, and Sports Officials.
- Training for Health Care Providers
- Concussion Videos
CDC "HEADS UP" Fact Sheets and More: Specific concussion information for coaches, parents, officials, and teen athletes.
National Association of School Nurses (NASN)
LOOKING FOR MORE INFORMATION? CHECK OUT THE HELPFUL RESOURCES TAB!
 CDC’s Concussion & Traumatic Brain Injury website featuring data, reports, and fact sheets.
CDC’s Concussion & Traumatic Brain Injury website featuring data, reports, and fact sheets.
CDC HEADS UP: Whether you are a parent, youth sports coach, school coach, school professional, or health care provider, this site will help you recognize, respond to, and minimize the risk of concussion or other serious brain injury.
Comparing Head Impacts in Youth Tackle and Flag Football. A CDC study published in Sports Health reports youth tackle football athletes ages 6 to 14 sustained 15 times more head impacts than flag football athletes during a practice or game and sustained 23 times more high-magnitude head impact (hard head impact).
Head impacts increase the risk for concussion and other serious head injuries.
Key findings from the study “Head Impact Exposures Among Youth Tackle and Flag American Football Athletes” include:
** Youth tackle football athletes experienced a median of 378 head impacts per athlete during the season.
**Flag football athletes experienced a median of 8 eight head impacts per athlete during the season.
These findings suggest that non-contact or flag football programs may be a safer alternative for reducing head impacts and concussion risk for youth football athletes under age 14.
CDC Pediatric Mild TBI Guideline consists of 19 sets of clinical recommendations. These recommendations are designed for all healthcare providers who care for pediatric patients with this injury.
Free CDC Provider Tools:
- School Letter: Returning to School After a Concussion
- CDC Pediatric mTBI Checklist;
- Diagnostic Recommendations
- Prognostic Recommendations
- Management & Treatment Recommendations
CDC Report to Congress: The Management of Traumatic Brain Injury in Children: Opportunities for Action
![]() Follow this link to access the TN Office of Coordinated School Health website.
Follow this link to access the TN Office of Coordinated School Health website.
 Follow this link to access the National Association of School Nurses website.
Follow this link to access the National Association of School Nurses website.